Much of life in the U.S. in the next year — our ability to send our kids to school, return to work fully and travel — depends on our ability to test, manufacture and distribute an effective COVID-19 vaccine. But while such a vaccine is universally needed, the virus has had a disproportionately heavy toll on some Americans.
The age-adjusted mortality rate from COVID-19 is more than three times higher for Black and Indigenous people than it is for white people and more than two times higher for Pacific Islanders and Latinos. By the end of April, 90 percent of predominantly Black communities were affected by COVID-19; by the end of June, 31 percent of Black Americans personally knew someone who had died of coronavirus.
In this time of hyper-visible conversations around health equity and racial justice, a persistent question remains.
In this time of hyper-visible conversations around health equity and racial justice, a persistent question remains: As we move with unparalleled speed toward a COVID-19 vaccine, will Black and brown people be left behind? Both our history and our present have set us on a trajectory to fail to deliver a vaccine to communities that need it most, through a combination of scientific abuses, systematic exclusion from both research and clinical care, and structural barriers to access to even basic health care.
The shadow cast by unethical human experimentation on communities of color is very long. From the unconscionable withholding of treatment from 600 men in the Tuskegee Syphilis trial to the exploitation of Henrietta Lacks in research, racism is built into the U.S. biomedical enterprise. And while these examples have become relatively well known, there are many others that have escaped the mainstream; further, racial inequities are not solely in our past. African Americans make up about 13 per of the U.S. population but on average make up 5 percent of clinical trial participants; Hispanic or Latinos make up approximately 18 percent of the population and only 1 percent of clinical trial participants.
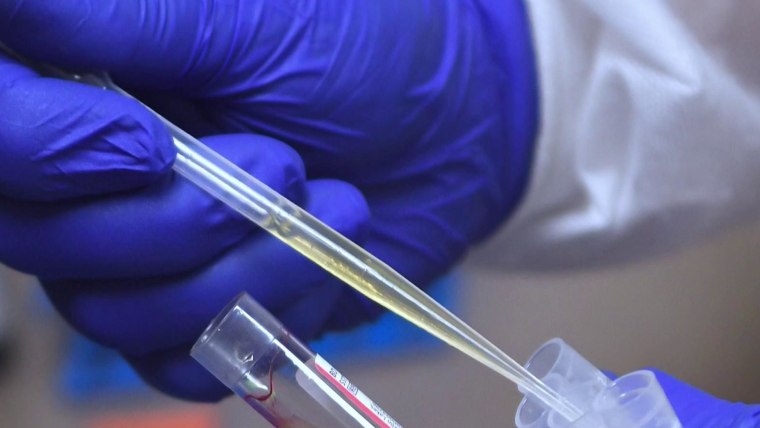
Similarly, current research has already failed to focus on populations disproportionately affected by COVID-19. Of the 45 participants in Moderna’s phase 1 clinical vaccine trial, the leading vaccine study in the U.S., six were Hispanic (13 percent), two were Black (4 percent), one participant was Asian (2 percent) and one was Native American (2 percent), which does not reflect U.S. national demographics, let alone the COVID-affected population. The study authors did not comment on the lack of racial/ethnic diversity as a study limitation.
The inequity echoes the lack of access to other key resources during the pandemic for Black, Hispanic and Indigenous populations, including diagnostic testing, supplies like personal protective equipment, and treatment. A study from the COVID-19 and Cancer Consortium published in July showed that Black cancer patients were about half as likely to participate in clinical trials of the drug remdesivir (which has demonstrated efficacy in shortening the time to recovery) for the treatment of COVID-19, compared to white patients.
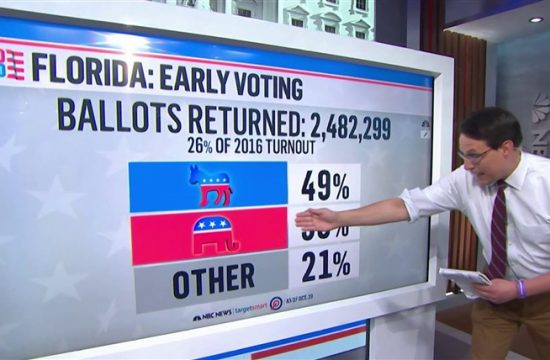
In an Associated Press/University of Chicago poll conducted in May, only 25 percent of Black Americans and 27 percent of Hispanic Americans said they would get the COVID-19 vaccine when one becomes available. In the context of the large gaps experienced in this pandemic, against a backdrop of historical medical abuses, the reluctance is understandable.
However, this hesitancy can become a convenient scapegoat for persistent health inequities. In fact, some research has demonstrated that lack of opportunity — not trust or attitudes about research — is the primary reason racial and ethnic minorities do not participate in clinical trials. What affects opportunity? Countless factors in the way that research is structured, including distance to established research sites, little effective outreach and messaging by study teams, a lack of culturally and linguistically appropriate recruitment materials, and other systemic factors that disproportionately exclude communities of color.
The complexity of this issue should not be used an excuse. Rather, it should serve as the motive for a concerted and prioritized effort. If a COVID-19 vaccine becomes widely available by early 2021, as many experts estimate, we have six months to get the will and the mechanisms in place.
To start, funders and regulators need to mandate balanced representation from diverse communities in clinical research on all vaccination trials, as well as studies of testing strategies and drug therapies, and require public disclosure when demographic targets for clinical trials have not been met. Journal reviewers and editors have a role in creating and communicating expectations for consistent, standardized reporting on targeted versus achieved demographic inclusion for published scientific studies. And all those actively engaged in conducting clinical research should take accountability for diverse representation in phase 3 trials.
If a COVID-19 vaccine becomes widely available by early 2021, as many experts estimate, we have six months to get the will and the mechanisms in place.
Researchers and public health agencies should disaggregate data on disease occurrence, hospitalization and death rates by race and ethnicity and make this data publicly available to inform priority areas for distribution. And they should create clear, transparent, publicly available metrics of equity for vaccine administration in every state.
Our elected officials and public health officials must also create a coordinated local, regional and national strategy for vaccine distribution that acknowledges and addresses potential barriers to vaccine dissemination among communities disproportionately affected by COVID-19. Residents and trusted leaders in those communities should play a central role in creating and executing such a plan and ensuring effective public messaging around it.
Communities of color cannot afford to be left behind as the government races aggressively toward a cure to this global pandemic. If we do not now design science and health care that benefits everyone, the enduring legacy of the pandemic will continue to be its terrible inequities.
The views expressed are the authors’ personal views and do not necessarily reflect the policies of Oregon Health & Science University.